Vestibular migraines, often overshadowed by their more well-known sibling, the classic migraine, present a unique challenge. They’re not just about head pain; they involve the vestibular system, responsible for maintaining balance and spatial orientation. Imagine the disconcerting feeling of dizziness, vertigo, and imbalance, coupled with or without the traditional migraine headache. That’s the reality for many living with this condition.
But why does this happen? What makes vestibular migraines tick? In this blog post, we’ll peel back the layers of this condition. We’ll explore what vestibular migraines are, the common (and not-so-common) symptoms, and the sneaky triggers that can set off this whirlwind. And because knowledge is power, we’ll also delve into the latest treatments, from lifestyle adjustments and supplements to alternative remedies that can help steady our shaky ground.
Just a quick note: I’m not a doctor, I don’t even play one on TV, but I am excited to share my personal low histamine diet journey with you because it has been life-changing for me. Remember, what works for me may not be a perfect fit for you. This blog is meant to share what I discovered through research and working with my doctors and hopefully offer some helpful insights based on my experiences. Before making any big changes, it’s always a good idea to chat with your healthcare provider.
UNDERSTANDING VESTIBULAR MIGRAINES
Introducing the Vestibular System
To understand vestibular migraines we need to understand the vestibular system. Imagine your brain as a busy control center that’s constantly receiving and processing information from all around your body. Now, one of the key departments in this control center is the vestibular system, which is like the team responsible for keeping you balanced and oriented in your environment. Your vestibular system is a part of the inner ear and brain that helps control balance and eye movements. It’s what helps you know up from down, left from right, and keeps you steady when you’re moving.
So What is a Vestibular Migraine?

A vestibular migraine is a type of migraine that specifically affects this balance system in your brain. When you have a vestibular migraine, it’s as if the signals that help you balance and orient yourself get mixed up. You might feel dizzy, have a sense of spinning (vertigo), or feel like you’re swaying or tilting even when you’re still. It’s like being on a boat in choppy waters, even though you’re just standing in your kitchen.
Unlike typical migraines, vestibular migraines don’t always come with a headache. Sometimes, dizziness and balance issues are the main problems.
VESTIBULAR MIGRAINE SYMPTOMS
The symptoms of vestibular migraine can vary widely but commonly include:
- Vertigo: This feels like you or your surroundings are spinning, creating a disorienting and often nauseating sensation.
- Dizziness: A general feeling of lightheadedness, unsteadiness, or a sense of floating, like you’re about to tip over.
- Balance Issues: Difficulty walking or keeping your balance, feeling like you might fall.
- Nausea and Vomiting: An uneasy feeling in the stomach that can lead to vomiting, often exacerbated by motion or spinning sensations.
- Motion Sickness: A heightened sensitivity to movement, where traveling in a car or even watching moving objects can cause discomfort.
- Sensitivity to Light and Sound: An overwhelming response to bright lights or loud noises, which can intensify symptoms.
- Tinnitus: Ringing or buzzing in the ears, which can be constant or come and go.
- Visual Disturbances: Experiencing visual disturbances such as flashes of light, floaters, or temporary vision loss.
- Headache: Although not always present, headaches can occur, ranging from mild to severe in intensity.
- Blurry vision: Difficulty focusing your eyes, and seeing things clearly. Can affect just one eye like it does for me.
- Ear fullness, pressure, or crackling: A feeling of stuffiness or blockage in one or both ears. Like having your ears plugged during takeoff on an airplane.
- Disequilibrium: A sense of instability (swaying, tilting, unsteady) while standing or walking, like walking on very soft sand or feeling like the ground is moving under your feet as if you’re walking on a gently rocking boat.
- Anxiety – Feeling dizzy, off-balance, or like the world is spinning can be unsettling and trigger a fight-or-flight response. Anxiety that feels like it is out of your control.
- Depersonalization – A feeling of detachment from oneself, often described as feeling like an observer of one’s own body or thoughts. It can be a disturbing and distressing experience, making you feel like you’re in a dream or watching your life from a movie screen.
- Derealization – Feeling like you have a distorted perception of the external world, making it feel unreal, distant, or even artificial like looking at your surroundings through a thick fog or a plastic window.
- Brain Fog – A temporary mental cloudiness, impacting focus, memory, and clarity, leaving you feeling mentally sluggish and forgetful.
- Fatigue – Feeling drained of energy, leaving you feeling physically and mentally exhausted, like you’ve run a marathon.
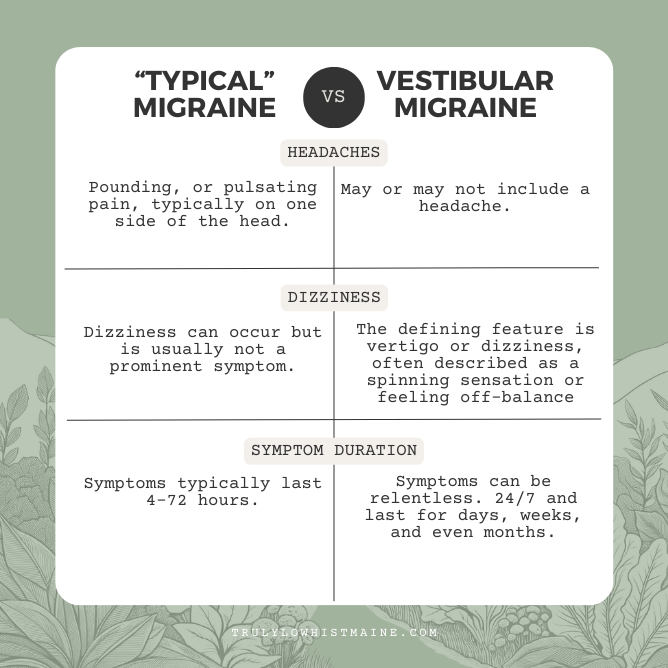
Differentiating Vestibular Migraine from “Regular “Typical” Migraines
While typical migraines are known for intense head pain often paired with light and sound sensitivity, vestibular migraines bring a different experience. Let’s highlight the key differences:
VESTIBULAR MIGRAINE TRIGGERS
While the exact cause of vestibular migraines remains a mystery, several factors can act as triggers, causing an attack or worsening existing symptoms.
- Diet: Certain foods and beverages, particularly those high in histamine, tyramine, or nitrates, can trigger migraines in some people. This can include aged cheeses, fermented foods, alcohol, caffeine, chocolate, and processed meats.
- Dehydration: Not drinking enough fluids can lead to dehydration, which can be a trigger for migraines.
- Hormonal changes: Fluctuations in hormones, particularly during menstrual cycles or (peri)menopause, can trigger migraines in some individuals.
- Stress and anxiety: Mental and emotional stress is a major trigger for many people with vestibular migraines.
- Sleep disturbances: Both irregular sleep patterns and insufficient sleep can increase the risk of vestibular migraine attacks.
- Medications: Some medications, such as some pain relievers and birth control pills, can trigger migraines in certain individuals.
- Sensory exposure: Bright lights, loud noises, strong smells, and flickering screens can all trigger vestibular migraines in some people.
- Motion sickness: Certain activities that involve motion, such as traveling by car, plane, or boat, can trigger dizziness and vertigo in individuals with vestibular migraines.
- Weather changes: Changes in barometric pressure or humidity can be triggers for some people with vestibular migraines.
Here are some additional factors to consider:
- Individual triggers: Everyone with vestibular migraines experiences different triggers, so it’s important to identify what specifically triggers your own attacks. This can be done by keeping a migraine diary to track your symptoms and potential triggers.
- Combination of triggers: Often, it’s not just one factor but a combination of triggers that leads to a vestibular migraine attack.
- Sensitivity: The same trigger may affect different people with varying degrees of severity.
VESTIBULAR MIGRAINE AND HISTAMINE CONNECTION
Emerging research points to the potential benefits of steering clear of certain foods to lessen both the frequency and severity of migraine episodes, vestibular migraines included.
Typical culprits in the diet that could trigger migraine attacks are foods like chocolate, alcohol, coffee, aged cheeses, and processed meats. These items are known to contain tyramine, nitrates, HISTMAINE, and phenylethylamine – all of which have ties to migraine symptoms.
Let’s Dig into the Histamine –> Vestibular Migraine Connection
Histamine’s Role: Histamine is a compound involved in the body’s immune response. It causes blood vessels to swell or dilate, allowing white blood cells to quickly find and attack infections or problems. This histamine buildup can lead to headaches and feelings of being flushed, itchy, and miserable.
Histamine Intolerance: If histamine is not properly broken down in the body, it can lead to histamine intolerance. This condition can cause headaches and other symptoms associated with migraines.
Impact on Vestibular Migraines: For individuals with Vestibular Migraines, consuming foods high in histamine can trigger or worsen their symptoms. These foods include citrus fruits, nuts, aged cheese, and others. Avoiding these high-histamine foods can help in managing Vestibular Migraines.
Dietary Considerations: A low histamine diet, emphasizes the importance of avoiding foods high in histamine and histamine-liberating foods to manage migraine symptoms. For a detailed dive into adopting a Low Histamine Diet, check out my blog post here.
So…let’s sum it up! Histamine plays a crucial role in triggering and exacerbating Vestibular Migraines. Managing histamine levels through diet, specifically by avoiding high-histamine foods, can be an effective strategy for controlling these migraines.
HEALTHCARE PROFESSIONALS FOR VESTIBULAR MIGRAINES
When vestibular migraines throw your world off balance, seeking the right healthcare professional becomes a crucial step toward regaining control. The expertise required is as unique as the condition itself, often necessitating a multi-disciplinary approach for effective management. Here’s a guide to the types of healthcare professionals who can play pivotal roles in your care:
- Neurologists: Specialists in the brain and nervous system, neurologists are often the go-to experts for diagnosing and treating migraines, including vestibular types.
- ENT Specialists (Otolaryngologists): These professionals specialize in the ear, nose, and throat, and can help determine if your symptoms are related to inner ear issues.
- Audiologists: They focus on hearing and balance disorders and can conduct various tests to assess vestibular function.
- Vestibular Rehabilitation Therapists: These are physical therapists specialized in treating balance disorders and can tailor a vestibular rehabilitation program for your needs.
- Dietitians or Nutritionists: Especially important if your migraines are linked to dietary triggers or histamine intolerance, these professionals can guide you in making dietary adjustments.
- Headache Specialists: These are neurologists or other physicians who have additional training and focus on the treatment of migraines and headache disorders.
- Psychologists or Psychiatrists: Given the emotional and mental toll chronic migraines can take, these mental health professionals can be crucial in helping manage the stress, anxiety, or depression that might accompany your condition.
- Functional Medicine Doctors: These practitioners take a holistic approach, looking at your lifestyle and environmental factors, and often delve into the root causes of conditions like migraines, offering personalized treatment plans.
Remember, building a relationship with the right healthcare professional is key. It’s about finding someone who not only understands the complexities of vestibular migraines but also empathizes with your journey, empowering you to manage your condition confidently.
TREATMENT AND MANAGEMENT FOR VESTIBULAR MIGRAINES
Once you identify your triggers, you can take steps to avoid them or minimize their impact. Somethings you can do today, right now to start managing your vestibular migraines, while, other things will require you to work with a healthcare professional.
LIFESTYLE CHANGES
Lifestyle changes you can make today to help manage vestibular migraines:
- Follow a dietary plan: Some people find relief by following a low-histamine or migraine-elimination diet.
- Stay hydrated: Drink plenty of water throughout the day. A good rule of thumb is to take half your body weight and drink that amount in ounces of water. More if you exercise.
- Maintain a regular sleep schedule: Aim for 7-8 hours of sleep each night.
- Use Stress management techniques: Practices like yoga, meditation, and deep breathing can help manage stress and anxiety.
- Join Community and support groups: Having a group of people, a community you can turn to when you have questions or just need to talk to someone who truly understands what you are going through and help with the stress and uncertainty of living with vestibular migraines.
MEDICATION, SUPPLEMENTS AND THERAPY
A healthcare professional can tailor a treatment plan uniquely suited to your needs. This plan may include a mix of medications to alleviate symptoms and prevent future episodes, supplements, and possibly vestibular rehabilitation therapy to improve balance and reduce dizziness.
Medications
To treat and manage vestibular migraines, healthcare providers often prescribe a combination of preventive, symptom-specific, and acute treatment options to alleviate symptoms during an attack. Please note, that this is not an exhaustive list, and it’s important to consult with your healthcare provider to determine the best treatment plan for your individual situation.
Preventive Medications: These are the cornerstone for those with frequent or severe episodes. Options include:
- Beta-Blockers (e.g., propranolol): Traditionally used for high blood pressure, they can also reduce the frequency and intensity of migraines.
- Antiseizure Medications (e.g., topiramate or valproic acid): Known for their use in epilepsy, they help stabilize nerve activity, which can be beneficial in preventing migraines.
- Calcium Channel Blockers (e.g., verapamil): Used for heart conditions and high blood pressure, they can also be effective in migraine prevention.
- Antidepressants (e.g., amitriptyline): While primarily for depression, some of these medications can help prevent migraines by influencing serotonin levels.
Acute Treatment Medications: For stopping a migraine in its tracks, these are often prescribed:
- Triptans (e.g., sumatriptan): Specifically designed for migraines, they work by constricting blood vessels and blocking pain pathways in the brain.
- NSAIDs (e.g., ibuprofen or naproxen): Over-the-counter anti-inflammatory drugs can be effective, especially when taken at the first sign of a migraine.
- Anti-nausea Medications: These can be crucial for those who experience severe nausea or vomiting with their migraines.
Symptom-Specific Medications: Tailored to individual symptoms of vestibular migraines:
- Antihistamines or Anti-Vertigo Medications (e.g., meclizine): These can help alleviate the dizziness and vertigo symptoms that are hallmarks of vestibular migraines.
Supplements
When managing vestibular migraines, you’ll find that supplements can play an important role. While not always a standalone solution, these natural allies can work in tandem with prescribed treatments to help ease symptoms and potentially reduce the frequency of migraine episodes. Remember, it’s crucial to consult with your healthcare provider before starting any supplement regimen, as the effectiveness and safety of supplements can vary, and interactions with other medications must be considered.
Most Popular Supplements Used to Manage Vestibular Migraines:
- Magnesium: Often hailed for its nerve-calming properties, magnesium may help reduce the frequency of migraines by regulating neurotransmitters and blood vessel constriction.
- Riboflavin (Vitamin B2): This vitamin is known for its potential to increase energy production in brain cells, which can be beneficial in reducing migraine frequency.
- Vitamin D: Vitamin D’s anti-inflammatory properties may help prevent migraines by calming inflammation, regulating neurotransmitters, and boosting magnesium absorption. While research is ongoing, Vitamin D could be a promising tool for migraine prevention, especially for those with deficiency.
- Coenzyme Q10 (CoQ10): Acting as an antioxidant, CoQ10 is thought to improve mitochondrial function and reduce inflammation, which can be helpful in managing migraines.
- Omega-3 Fatty Acids: Found in fish oil supplements, these fatty acids are known for their anti-inflammatory properties and may help in reducing the frequency and severity of migraines.
- Feverfew: A traditional herbal remedy, feverfew has been used for centuries to treat headaches and is believed to have properties that can mitigate migraine symptoms.
- Butterbur: The natural chemical compounds found in butterbur roots, known as petasins, are the key players that make this herbal remedy highly effective for migraine prevention. Petasins work by modulating the body’s pain response and reducing inflammation, thereby playing a significant role in mitigating migraine symptoms.
- Ginger: This culinary mainstay isn’t just a flavor bomb; it’s a natural triptan that may treat pain and nausea associated with vestibular migraines.
- Melatonin: Known primarily for its role in regulating sleep, melatonin may also help in reducing migraine frequency, particularly in individuals with sleep disturbances.
Vestibular Therapy
In the challenging world of vestibular migraines, vestibular therapy emerges as a highly effective and empowering treatment approach. It involves a series of customized exercises, guided by skilled vestibular therapists, aimed at retraining the brain to correctly interpret and respond to signals from the inner ear, thereby improving balance and reducing dizziness. This therapy not only focuses on immediate symptom relief but also on long-term management strategies, helping individuals adapt to and cope with their symptoms more effectively. Through a combination of balance training, gaze stabilization, and habituation exercises, vestibular therapy can significantly enhance one’s quality of life, reducing the disorienting impact of these migraines. I had incredible success with the Dizzy and Vertigo Institute of Los Angeles.
ALTERNATIVE THERAPIES
Alternative therapies offer diverse and often holistic methods to complement traditional treatments, focusing on overall wellness and symptom management. Below are some alternative therapies that have shown promise for those dealing with vestibular migraines.
- Acupuncture: This ancient technique involves inserting fine needles into specific points on the body, aiming to restore energy balance and potentially reduce migraine symptoms. While the exact mechanism isn’t fully understood, acupuncture may regulate the autonomic nervous system and modulate the balance of neurotransmitters involved in vestibular function
- Yoga and Tai Chi: These mind-body practices combine physical postures, controlled breathing, and meditation to promote relaxation and stress reduction. Stress is a well-known trigger for migraines, so by calming the mind and body, these practices may help lessen the frequency and severity of attacks. Additionally, balance and coordination training in some yoga and Tai Chi poses can benefit the vestibular system.
- Biofeedback: This technique uses special equipment to monitor bodily functions like heart rate, blood pressure, brain waves, muscle tension, and skin temperature. The patient then learns to control these functions through relaxation techniques and mental focus. Biofeedback can help individuals identify and manage early warning signs of a migraine, potentially preventing the full attack. It can also help manage anxiety and stress, which can contribute to vestibular migraines.
- Aromatherapy: Utilizing essential oils like lavender or peppermint, aromatherapy can provide symptomatic relief, especially for nausea and dizziness associated with vestibular migraines.
- Herbal Remedies: Natural supplements such as feverfew and butterbur are traditional remedies for migraine relief, but require consultation with a healthcare provider for safety.
- Massage Therapy: Regular massage sessions can help alleviate stress and tension, common triggers for migraines, while also improving circulation. While research is mixed on its specific effectiveness for vestibular migraines, some individuals report relief from massage sessions.
- Chiropractic Care: Some people find relief from migraine symptoms through chiropractic adjustments, which aim to realign the spine and improve nerve function. While research on the effectiveness of chiropractic care for migraines is mixed, some individuals report reduced frequency and severity of attacks after receiving regular adjustments. It’s important to consult a qualified chiropractor with experience in vestibular migraines.
- Mindfulness and Meditation: Mindfulness and meditation can help reduce stress and anxiety, both of which contribute to migraines. By promoting relaxation and self-awareness, these practices may help individuals manage their migraine triggers and lessen the impact of attacks. Calm or Headspace are great apps to help with this.
- Migraine Glasses: Specially designed glasses that filter out harmful light can significantly reduce light sensitivity and discomfort often associated with migraines. Avulux and Therspecs are two brands worth looking at.
- Green Light Therapy: Exposure to a specific wavelength of green light has been found to reduce the severity and frequency of migraines for some people, offering a novel and non-invasive option. Check out the Ally lamp for this.
- Binaural Music: Imagine two slightly different tones, one played in each ear, creating a perceived sensation of a single beating tone at the difference in frequency. Specific binaural beats, particularly within the theta range (4-8 Hz), have been linked to reduced migraine pain and frequency.
- Salt Water Sole: A solution of Himalayan salt dissolved in water, consumed in small amounts, is believed by some to provide electrolyte balance and hydration, potentially aiding in migraine management. In addition to electrolytes and hydration, the solution contains minerals like magnesium and calcium. However, there is potential health risks associated with consuming high amounts of sodium. Talk to your doctor before trying this therapy.
Remember, these alternative therapies may not be effective for everyone, and some may require further research to confirm their benefits for vestibular migraines. Consulting your healthcare provider is crucial to determine which approach might be right for you, considering your individual needs and medical history. Additionally, combining alternative therapies with traditional medication and lifestyle modifications may provide the most effective management approach for vestibular migraines.
RESOURCES AND TOOLS
These are the books, websites, and apps that are helpful resources for learning about and managing Vestibular Migraines.
Books
Heal Your Headache: A book that helps you manage your migraines by reducing your triggers. The main focus being on introducing a migraine diet that eliminates food triggers, and raising your migraine threshold.
Dizzy Cook Cookbooks: These cookbooks, using the guidelines of the Heal Your Headache diet, provide delicious recipes that make you forget you’re following a restricted diet.
Websites
The Dizzy Cook: There is so much value in finding someone who has already been through what you are currently going through. They can provide wisdom and hope in a time that can be very challenging. This is exactly what makes The Dizzy Cook so wonderful. She shares amazing migraine-friendly recipes and is a wealth of knowledge and hope for people living with vestibular migraines.
Migraine Strong: If you suffer from any form of migraine, this is the website for you. If you need migraine questions answered, Migraine Strong is a great place to start your research and may be the only place you need to go to answer that question.
Apps
Migraine Buddy: Migraine Buddy is a migraine-tracking app that helps you track your attacks, potential triggers, and what you did to get relief. It’s impossible to see the patterns when you don’t track them. This app allows you to see and find correlations between what triggered an attack and what seems to be helping to reduce the frequency or intensity of an attack.
Waterllama: Dehydration is a trigger for vestibular migraines, so keeping track of your water intake is vital in making sure you hit your daily water goals. Waterllama is an app that makes it fun to track your water intake and helps you create a habit of drinking water.
Headspace or Calm: Headspace and Calm are excellent tools for practicing mindfulness and meditation, helping to reduce stress which is a known migraine trigger.
Social Media Accounts
The Dizzy Cook: Referenced above for her Website and cookbooks, you can follow The Dizzy Cook on Facebook and Instagram.
Bobby Parish: Bobby is a go-to source for people seeking cleaner, more wholesome food options. He takes you along to grocery stores where he reviews food labels and lets you know which products are “Bobby Approved” – products that meet his standards for clean and nutritious eating. You can follow Bobby on Instagram, Facebook, and YouTube.
VESTIBULAR MIGRAINE FAQ
What helps vestibular migraines?
Managing vestibular migraines often involves a combination of approaches: medications prescribed by healthcare professionals, lifestyle modifications like stress reduction and dietary changes, and vestibular rehabilitation therapy for balance issues. Additionally, supplements such as magnesium and vitamin B2, along with alternative therapies like green light therapy and yoga, can complement traditional treatments. Each person’s response varies, so it’s essential to work with a healthcare provider to tailor a plan that suits individual needs.
What Triggers Vestibular Migraines?
Vestibular migraines can be triggered by various factors, including stress, dehydration, hormonal changes, certain foods and additives, irregular sleep patterns, and sensory stimuli like bright lights or loud noises. Environmental factors, such as weather changes or motion sickness, can also play a role. It’s important to note that triggers can vary greatly from person to person, making individual assessment crucial for effective management.
What does a Vestibular Migraine Feel like?
The most defining symptom is dizziness and vertigo: a feeling of spinning, swaying, or tilting. This can range from mild unsteadiness to the room feeling like it’s swirling around you. Nausea often follows, and you may feel like you might vomit. Other common features include balance issues where you are feeling off-kilter and/or unsteady, tinnitus (ringing in the ears), light and sound sensitivity, blurry vision, and brain fog.
The mix and severity of these symptoms can vary from person to person and across different attacks. In some cases, there may be a throbbing headache like a typical migraine, but not always. It’s a disorienting and unpleasant experience, making everyday activities feel like a challenging obstacle course.
How long can Vestibular Migraines last? Can Vestibular Migraines last weeks? months?
The duration of vestibular migraines can vary significantly, ranging from a few minutes to 24 hours a day, every day, for months. The frequency and length of episodes differ greatly among individuals.
Who treats Vestibular Migraines?
Vestibular migraines are typically treated by audiologists specializing in the vestibular system, and/or neurologists, who specialize in brain and nervous system disorders. In some cases, ENT specialists (otolaryngologists) may also be involved, especially when inner ear issues are suspected. Additionally, vestibular rehabilitation therapists can provide specialized physical therapy to help manage balance-related symptoms. It’s important to have a multi-disciplinary team for comprehensive management of this condition.
What Causes Vestibular Migraines?
Vestibular migraines are believed to be caused by a combination of genetic and environmental factors leading to abnormal brain activity. Specific triggers can vary, but they often include stress, certain foods, hormonal changes, and sensory stimuli like bright lights or loud noises. The exact mechanisms are still not fully understood, and research is ongoing to uncover more about the causes of this complex condition.
Why am I suddenly getting vestibular migraines?
The sudden onset of vestibular migraines can be due to various factors, including changes in stress levels, hormonal fluctuations (such as those associated with menstruation, pregnancy, or (peri)menopause), alterations in sleep patterns, or dietary changes. It’s also possible that you’ve always had a predisposition to vestibular migraines (especially if you have a history of migraines), and recent lifestyle changes or environmental triggers have now brought the symptoms to the forefront. Consulting with a healthcare professional is crucial to accurately diagnose and understand the specific causes of your case.
SOURCES
Vestibular Migraines: Johns Hopkins Medicine
Vestibular Migraine: Cleaveland Clinic. Published August 29, 2023
What to Know about Vestibular Migraine: American Migraine Foundation. October 5th, 2020
Vestibular Migraine Symptoms: Alicia Wolf. The Dizzy Cook. Published June 7th 2022
How to Follow a Vestibular Migraine Diet: Ryan Ramen Medically reviewed by Heidi Moawad, MD. Healthline. Published August 21, 2023
What Is The Heal Your Headache Diet?: Alicia Wolf. The Dizzy Cook. Published March 21, 2020
Heal Your Headache: The 1-2-3 Program for Taking Charge of Your Pain by David Buchholz and Stephen G. Reich Published January 15, 2019
The Vestibular Migraine Treatments That Cured My Daily Dizziness: Alicia Wolf. The Dizzy Cook. Published June 14, 2022
Natural Supplements for Vestibular Disorders: Alicia Wolf. VEDA.
How to calculate how much water you should drink: Jennifer Stone, PT, DPT, OCS, Clinic Supervisor. University of Missouri System
5 Vitamins and Supplements for Migraine Headaches: Lizzie Streit, MS, RDN, LD — Medically reviewed by Grant Tinsley, Ph.D., CSCS,*D, CISSN, Nutrition. Published March 24, 2023